Choosing the best probiotic for C. diff.
Other Categories
Guest Blog by Lynne V. McFarland, PhD
Choosing the best probiotic is not an easy task. There are over 250 different types of probiotic products found on the market (grocery stores, pharmacies, on-line websites, etc.), but relatively little guidance on how to choose one probiotic over another. As more research is done, the guidelines of how best to use probiotics continue to be updated.
This post is to help you choose a good probiotic for what you need-either to prevent you from getting a C. difficile infection after exposure to antibiotics or to prevent a recurrence of C. difficile infection after you have  recovered.
recovered.
Why should I consider using probiotics to prevent C. difficile? Probiotics are living microbes that are especially beneficial when the normally protective microbiome has been disrupted. C. difficile infections occur after your normal gut microbes have been disrupted, typically after you have been given antibiotics to treat an infection.
How does bacteria in my gut protect me? Normally, the “good” bacteria in your gut protects you from disease-causing organisms. In addition to digesting your food, your normal microbiome (all the different types of microbes in your gut) also form a protective barrier that repels disease microbes. However, this protective barrier can be disrupted. Taking antibiotics is the major culprit in killing off your good microbes. Once this happens, disease-causing microbes use this opportunity to infect your gut. You are now susceptible to infection.
Why doesn’t everyone who gets antibiotics come down with C. difficile? The type of antibiotic and other factors (age, other medications, other current diseases) can make you more or less likely to be infected with C. difficile. But you also have to be exposed to C. difficile. Once exposed to C. difficile spores (either already in low numbers in your gut or from external sources like other patients or room surfaces in healthcare facilities), these inactive spores germinate (like seeds sprouting) and C. difficile infects your gut. Once C. difficile sets up housekeeping in your gut, it produces toxins that cause inflammation and diarrhea.
How can probiotics help? Some types of probiotics can reduce the inflammation caused by C. difficile, some can kill the C. difficile bacteria directly, some can prevent C. difficile from attaching to your gut surface and some can destroy the toxins that cause the diarrheal symptoms. Only certain types of probiotics can be helpful in preventing C. difficile infection.
Aren’t all probiotics alike? No. Recent research has found that how well a probiotic works is different by the type of disease it is being used for (called ‘disease-specificity’) and that the choice of probiotic strain is important (called ‘strain-specificity’). Some types of probiotics are useful against C. difficile, while many are not effective.
How do I know what strain or strains are in a probiotic product? The label on the probiotic product should list all the microbes (bacteria or yeasts) contained in that product. Each microbe has a three-part name: the genus (for example, Lactobacillus), the species (for example, acidophilus) and the strain (for example CL1285). As an example, a border collie is scientifically named as: Canis (the genus) lupus (the species) familiaris (the strain). Just as not all dogs are like collies, not all Lactobacilli are alike.
If it says ‘probiotics’ on the label, can I use this for C. difficile? Not all the products found on pharmacy shelves fulfil the definition of probiotic. The World Health Organization defined probiotics as living organisms that have an adequate dose and show a health effect. This means the probiotic is alive (can be a bacteria or yeast), must have a good number of organisms (dose) and shows an effect on health. Typically, effectiveness is shown by doing a clinical trial. Not all types of probiotic products on the market fulfill even these three simple requirements.
Why aren’t the labels more helpful in choosing a probiotic? In the United States, most probiotics are sold as ‘dietary supplements’ available over-the-counter and can only have health claims on their labels, which give no specific guidance on how to use the probiotic for a specific disease or illness. Because dietary supplements do not go through the rigorous FDA approval process as do prescription medications, your physician is not the usual role of recommending your medication. The choice is left open to you as an individual. Dietary supplements, by law, can not claim to ‘treat’ or ‘cure’ a disease.
How should I choose an appropriate probiotic? One way is find a scientific review that provides you guidance on which probiotics are best. I have listed a few good practical guides below.
- Sniffen JC, McFarland LV, Evans CT, Goldstein EJC. Choosing an appropriate probiotic product for your patient: An evidence-based practical guide. PLOS One 2018 Dec 26;13(12):e0209205. [doi: 10.1371/journal.pone.0209205., PMID:30586435]
- McFarland LV. From Yaks to Yogurt: The history, development and current use of probiotics. Clin Infect Dis 2015; 60(S2):S85-S90. [doi: 10.1093/cid/civ054, PMID: 25922406]
Five tips for choosing a probiotic.
Another way is to look for these five tips of what a good probiotic product should have on the label (see box). If the probiotic doesn’t meet all five criteria, you should just put it back on the shelf and choose another probiotic.
- FDA Disclaimer. All dietary supplements (including probiotics) are required to have an FDA disclaimer on the label. “FDA Disclaimer: The FDA has not evaluated this claim. This product is not intended to cure, mitigate, treat, diagnose or prevent a disease.” Does your product have this disclaimer? If not, put it back.
- Which strains? Does the label list each strain of bacteria or yeast that is present in the product? Some products just say “A Probiotic”, but do not list which strain or strains are present. If no listing of each strain is given, don’t buy it.
- Dose. Is the daily dose or concentration given on the label? This is usually listed as “number of cfu” (colony-forming units or number of organisms). The number of bacteria or yeasts should be at least 5 billion per day. If the probiotic gives no dose information, don’t buy it.
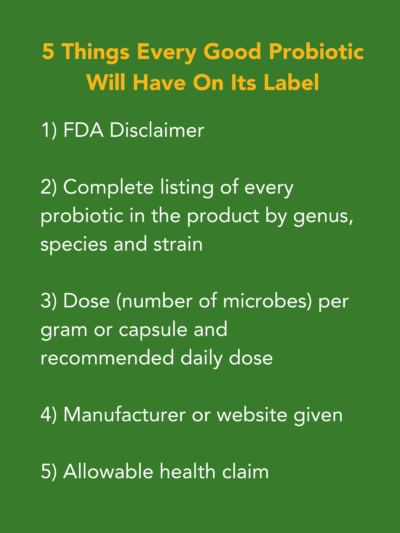
- Who made the probiotic? A reliable manufacturing company should have a history of producing a high-quality product and is certified by the appropriate authority. If there is no information on who made the product, you should be suspicious. Although not required by law, most reputable probiotics list a website or source for more information. This can be helpful for you to see if there are good clinical trials that might support their claims for a health benefit.
- Health claim. Dietary supplements are allowed to make ‘structure or function claims’ by law. Allowable health claims include “boosts your immune system” or “strengthens your intestinal function”. If the product claims that it ‘cures cancer’ or ‘treats diseases’, don’t buy it.
Because of the current FDA regulations for dietary supplements, you should not find any probiotics in the US claiming to treat or cure C. difficile infections. However, in the future some probiotics may be granted permission to say this if they are approved by the FDA as a medication or medical food. Other countries have different regulations that also may allow them to state different claims for their probiotic.
How do I know which probiotics can be used to prevent a C. difficile infection? Fortunately, there is over 35 years of research done in different countries with clinical studies and randomized controlled trials that have shown which probiotic strains are effective for different types of diseases. In 2020, the American Association of Gastroenterology recommends four probiotics to prevent C. difficile infections after antibiotic exposure, but five others types of probiotics were not found to prevent C. difficile infections. Only two of the probiotics had multiple trials to support this claim: Saccharomyces boulardii CNCM I-745 [Florastor®, Laboratories Biocodex] and a three-strain mixture of L. acidophilus CL1285 + L. casei LBC-80R + L. rhamnosus CLR2 [Bio-K+, Bio-K PLUS International].
When should I start taking the probiotic to prevent C. difficile infection? The probiotic should be started as soon as possible after the antibiotic is started (best within 24 hours) and continued while you take your antibiotic course and then for at least 2 weeks after the antibiotic is stopped to allow your normal gut microbiome to be restored. This combination (giving probiotic with antibiotic) has been tried in over 10 hospitals and has reduced their overall hospital rates of C. difficile significantly with no apparent side-effects.
If I’ve already had at least one episode of C. difficile, are probiotics useful to prevent further recurrences of diarrhea? About 1 of 5 people with one episode of C. difficile infection will develop at least one more episode (recurrence). Two clinical trials have shown when S. boulardii CMCM I-745 is given along with standard antibiotics to treat C. difficile infections, the recurrence rate is significantly reduced, especially if a high dose (2 grams/day) of vancomycin is given. The probiotic should be started at the same time of the vancomycin and continued for at least four weeks to allow the normal microbiome to become restored.
Are probiotics safe to take? Evidence from carefully monitored clinical trials has not found serious adverse reactions or side-effects for the probiotics described above. Generally, probiotics have been safe to take, reflecting the long history of clinical and safety trials. However, probiotics are generally not recommended for severely ill patients with central catheters.
To summarize, remember that just because a product says it is a ‘probiotic’, does not necessarily mean it is one. Also, not all probiotics are effective for the same type of health effect, so it is important to link the type of probiotic with the health effect that you need.
Lynne V. McFarland, earned her PhD in Infectious Disease Epidemiology at the University of Washington in Seattle in 1988 documenting how C. difficile was spread in the hospital. Since then, she has continued her research in C. difficile and branched out into the field of probiotics. She has published over 160 articles in scientific journals, is on the editorial board of several journals and has reviewed papers on probiotics and C. difficile for over 50 journals. She also has co-authored two books on probiotics including “The Power of Probiotics by Gary Elmer, Lynne McFarland and Marc McFarland”. She worked as a scientist for the Veteran’s Administration and as an affiliate associate professor at U. Washington, Seattle. She currently is active with the Public Health Reserves Corps fighting the COVID pandemic.




I am so grateful for this post! I was unsuccessful in researching which product (other than Florastor) contained the recommended probiotics, and this blog provided the answer and much more. Thank you!!!
Glad I came across this info. Diagnosed w cdiff without toxins yesterday. Started vancomycin but would like to get a yogurt that has probiotics that can help ease discomfort..Can you please recommend a yogurt? There are so many and I’m confused.
Thank You
Here are a couple of ideas from when I had c. diff: Dairy-based anything killed my gut. I opted for Silk almond milk yogurts and/or So Delicious coconut milk yogurts. So Delicious at least includes the probiotic strains. Califia also has a smoothie, though it’s not as readily available. I added a mild tasting miso to a lot of foods too. Try Bio K if these don’t work out. They do officially sell through Amazon now, but their website has a search tool to find places that sell it. Feel better!
My gastroenterologist recommends Kefir is better than yogurt for probiotics.
My GI recommended Kefir also but it hurt my insides too much so I couldn’t drink it.
Kefir causes significant itching in my wife and I. The oat based kefir has not caused itching so far for myself.
What is the best probiotic to take for c diff
There are 4 specific probiotics that i heavily researched and they stabilized/healed my gi after Vanco treatment. Saccharomyces boulardii CNCM 1-745 (Florastor) =aprox. $20 for 20ct/Walmart or Amazon.
L.plantarum 299v (Ideal Bowel Support by Jarrow Formulas) =aprox. $19 for 30cap/their website.
Lactobacillus rhamnosus GG (Culturelle) =aprox.$22 for 30cap/Walmart.com
Lactobacillus reuteri DSM 17938 *sometimes called, L. reuteri Protectis (BioGaia) =aprox.$25 for 30cap or chewable tabs/Amazon or Walmart.com
Also, drink kefir, eat Kimchi and eat Sauerkraut, yogurt helps too. I was depressingly desperate to fight this crap. I did all of the above, every single day. I nearly gagged but i didn’t care, I will never go through this again. I’m staying on this regimen for 3 months, to ensure this awful illness doesn’t come back. It’s costing me so much money but idc. I am a naturally very healthy female w/no comorbidities. I literally never get sick from anything, ever. I believe my blood work and stool tests came back so perfect (other than positive for C Diff), because I take so many vitamins daily and drink bone broth. i stay on top of my immune health. That’s probably why I didn’t have high WBC’s or Calprotectin and my Pancreatic Elastease was high-which it’s supposed to be if you’re healthy. Clindamycin wrecked it; that’s what killed my gut flora and made me so sick. My podiatrist fixed an ingrown toe nail, then it didn’t heal properly, so instead of doing a culture to see exactly what kind of bacteria she was treating me for, she just willy-nilly gave me 2 different types of anti-biotics. That fixed the toe and killed my gi. I’ve spent about $1,200 so far, buying all this stuff to repair my gi. I’m sure it’ll be a good $3,000 by the time it’s over n done. The Vanco was $800 for a 7 day treatment, then all the special foods, probiotics and shipping fees.
Good Luck! I hope that helps.
Lorraine, what was your prescribed dose of Vancomycin?
This is what worked for me and one other person who recommended it.
It has micro organisms found in some yogurts so i expect they are very safe.
Trader Joe’s Super acidophilus complex with intestinal delivery system 10 Billion organisms per tablet
Micro organisms per label
L. acidophilus 70%
L. rhamnosus 10%
B. biphidum 10%
B. longum 10%.
It cost about $12 in 2105
I only used about 5 out of 60
symptoms relief in one day but continued taking for 4 more days.
Intestinal delivery means it has coating for protection against stomach acid. I took it on an empty stomach with water.
@Star I am having the same complications from Clindamycin! I will be trying that exact probiotic along side kimchi, sauerkraut, kefir & whatever else I can find to naturally heal from this crap. I don’t want to do another antibiotic tbh considering this one caused it & I like to do things naturally anyways. But thank you your comment helped a lot!
I’ve had c diff 3 times back to back. My GI recommends florastor and 3 yogurts a day. Be on that regimen the rest of my life. Been on it since 2016.
Activia.. it says on label that it has thousands of probiotics
I never found activia to help with cdiff.
My GI said you’d need to eat six a day to get the same benefit of one probiotic.
That may be because it has a high sugar content which helps C diff grow!
Just came off around of antibiotics. Started taking Visbiome as a preventative. Most studied and concentration of microorganisms
I had a fecal transplant in 2015 after a 5 month battle with c diff. It saved my life. I recently had a dental procedure that required 7 days of amoxicillin…..I’m terrified. Have been taking florastor and will now increase the amount I take.
Hi kathleen, So I had my first recurrence of C. Diff infection,may I know if you have been prescribed of Dificid?
And I am thinking of fecal transplant just in case second recurrence occur, but I am terrified. Will you tell me please the procedure of how it is done?
Your reply would be greatly appreciated.
Thank you
Kathleen, i am 41 and on my 1st cdiff recurrence, I asked for a fecal transplant and doctor said I wasn’t a good candidate because I’m otherwise healthy… (?) Can you share some details please? Thank you!
She will do virtual visits and mail in dry ice your FMT TO YOU !
Dr Carmen Campbell 2240 N Interstate Ave, Suite 200 Portland, Oregon 97227 Email: info@drcarmencampbell.com Call: 503-908-4813
Hi how did you do? I had a FMT 3 years ago and started antibiotics Ammox today for an ear infection ugh
So the FMT worked,that’s fantastic, this is my third cdif infection in less than a year
Similary experience, now faced with taking antibiotics for bacterial infection. How did you fair with the antibiotics? Was there a cdiff reoccurrence? (My worst nightmare).
Does insurence cover fecal transplant?
Same here…did the c diff reoccur? I’m so scared to take the antibiotics!!
Is culturelle ok to take with antibiotics for cdif? Or do i need something different?
I have this question also. This is my third back-to-back occurrence of C diff…I can’t seem to get rid of it. I was on Vanco twice (both for 10 days) and now on Dificid (10 days) and Culturelle (health and wellness) daily. I wasn’t given a diet – they said I could go back to my normal diet…I really think something needs to change but I’m not the doctor:-(
Try Kefir
Also, I was just prescribed dificid for my c diff recurrence. Pharmacy is ordering it. I am trying to look for a good probiotic to take with it, apparently saccharomyces boulardii is the best, but I don’t know the brand, dosage etc.. I also have IBS-C. I had also been advised by gastro not to take probiotics because of preciously having SIBO which was succesfully treated with xifaxan.. any help is appreciated.
She will do virtual visits and mail in dry ice your FMT TO YOU !
Dr Carmen Campbell 2240 N Interstate Ave, Suite 200 Portland, Oregon 97227 Email: info@drcarmencampbell.com Call: 503-908-4813
58 yo male, just had shoulder surgery which included an IV dose of antibiotics. I now seem to have c.diff going on 3 weeks.
Is it feasible I can knock this out with Florastor, yogurt, ext? Or is it likely I’ll need antibiotics?
Starting Florastor today.
I had c diff after shoulder replacement. 2nd bout. This time was put on vancomycin. My doctor had me start Florastor. It wasn’t as severe as the first time, but he still recommended treatment. Hope this helps.
My family doctor never told me how contagious cdiff is. He treated it like a small stomach bug. Was on antibiotics for 1 yr and 3 months before a FMT stopped the symptoms.
Vancomycin is the only thing that helped me.
I started Florastor after suffering 2 weeks with C. Difficile after taking Clindamycin
And being hospitalized for low electrolytes. I’m noticing a calmness in my stomach/bowels. I was told to drink milk without lactose since when you have C. Diff. It is difficult for your stomach to process lactose.
activia is great!
I am on Vancomycin for two months now, as I previously took for 10 days 10ml a day, it helped for a while and them came back, recurrence had to take Vancomycin for longer period I hope the bacteria dies…
I did the same regiment and then had to use Dificid. It worked like a charm. It’s very expensive,
That’s why they have you take the vancomycin first, but there is Patient Assist through Merk the manufacture of Dificid (if you qualify)
My cost for the Dificid
With my insurance was $1400 but I was able to use the patient assistance program. I’ve had six bouts with the c-diff since October 2021. I
I am close to doing a bowel transplant. You can look up what that entails on the Internet.
I also take Florastor probiotic
I was hospitalized for 5 days with C-Diff was sent home for 5 more days with vancomycin prescription 4 times a day. Once I was done with meds, it re-occurred 2 days later, I was beside myself, got a prescription for vancomycin again for 40 days starting with 4 a day for 10 days, then 3 for 10, 2 for 10 and finally 1 for ten, I’m getting close to the end and am Petrified. Started drinking kefir, have been taking yogurt and culturelle all along. I Pray that it works if not I will go the other route
Obviously a “paid” comment, otherwise Susan would have mentioned what “product” contained the answer. …moving on to find it myself by calling my neighbor doctor.
Hi Sebastian, it’s not a paid post. Florastor is probably the best known probiotic. I would assume Susan didn’t mention what she used because it is something that should be decided with your doctor.
Are there certain foods that we should avoid when u have c did
Happy that I found this site
I used Florine 3 and drank kefir milk 3 times a day
I battled c diff for 3 years and ONLY after I found out about Florastor did it finally go away for GOOD! I swear by it and took it for years actually as a precaution. After 3 years of being infection free I finally stopped and switched to a basic probiotic.
Please let me know what probiotic you got is called just Florastor can you buy it at wal mart they have so much on the shelves so confusing. Thank you
This is Florastor’s website. You can buy their probiotics there or they also list where to buy in stores near you.
https://florastor.com/products/florastor/
Amazon sells Florastor
Walgreens has Florastor. I’ve been taking it since my first bout. Relapsed a few days ago and am now on Dificid. Researched some more and ordered HU58 bacillis subtilis. Anyone know if that is effective against c diff?
Can you help me???
I too am battling c diff. I am taking Florastor 150 mg morning and 150 mg evening. Is that the correct dose to fight c diff? I don’t want to keep having it. I got it because I had antibiotics when I had a tooth extracted. Thank you for your suggestions.
How often did you take Florostor? And what did you switch to? Thank you.
My son and I both got cdiff in March 22. Still recovering. Took 3 rounds vancomycin and now starting Florastor. Is it best to take the higher dosage of 4 pills a day or maintenence dose of 2 pills a day?
Thanks for the info. I just did a 10 day run with Vancomacin. My doc didn’t tell me to take a probiotic during treatment. I just started Florastor. I’ll stay on it for life at this point. How do I replace my gut biome? What a nightmare!
What probiotic have you used. I am just beginning recovery for my second C Diff infection. My daughter in law has had C Diff and was told to take Florastar and I was wondering if it was necessary for me to take such an expensive one.
What did you use? I have been taking florastor for a long time and just got cdiff back.help
Got cdiff 6 months ago. Take Florostor every day. Need to take a topical antibiotic for toe infection. Will topical cause relapse
I got C Diff (027 strain) in N.Thailand. I had not taken an antibiotic for years. My cleaning person admitted to being ill for days, but she gave me water every day. I got C Diff, likely from Spores. Worked for Govt, so stayed..went to the Hospital for three days, then realized, I was getting worse. I was 62 years old, a Vegetarian, no liquor ever, no co morbidities. Had C Diff in US, for 6 mos, until I resourced it.No one imagined it, as no antibiotic involvement.
Took five complete rounds of antibiotics, joined 5 Govt Studies…then got an FMT by Colonoscopy. Was 100% better, just hours after the procedure. But I got Tinnitus from the meds pretty bad, but my Gut Biome replicated to my 15 yr old donor’s biome…making mine 2.0! Been on probiotics ever since, developed with specificity by a Nutritionist. Try and get an FMT.
Thanks for your article. I am currently taking Align along with dificid for a reoccurrence. Is this a good probiotic.i am 68yrs old.
I have had a 2nd recurrence and when reordering Align from amazon, I found for about the same cost there is an Align 5x extra strength which seemed to help after completing Dificd and back on Vancomycin and awaiting Rifaximin
I had a very severe case of Cdiff Christmas 2018, I recovered after I was giving Flagyl and a round of probiotics however before the three rounds of Clyndamyacin that kicked in the Cdiff three months in a row, I’m lucky to be alive! I had another issue last month about four weeks ago or so with a dental infection again, this time they gave me amoxicillin, I started a probiotic and continue to take it, I get severe anxiety so I was only taking one a day and sometimes I wasn’t even taking that I was taking a child’s probiotic to help keep me regular as well. None of that was good enough added with the Activa yogurt. I think it kept it at bay so far but I can tell this morning that I am suffering. I’m going to go to the pharmacy this morning and pick up what is suggested, they gave me an off brand of floor store and that’s what I was rarely taking had I’ve been taking it the way it was intended one in the morning and one at night, I would’ve had a better chance of not having any issues at all. I noticed after I take it about an hour or two later I feel a little better I know that sounds weird but maybe it’s helping. Thank you for the article! God bless and I hope everyone stays healthy.
This is SO helpful! I have yet to find a brand of probiotics that works well for me, and as you mentioned, there’s not much guidance out there for us c diff patients. Thank you for providing this resource!!
My sister has just been diagnosed with c-diff. What is the best probiotic for me to get for her please.
Hi Mary, we generally cannot recommend specific products, but we have heard good things about Bio-K Plus from a couple of our Advocates.
Watch out with Bio K! I KNOW I developed an enterococcus infection from it. This strain is present, but not listed!!
I have cdiff this is my 5 time in 8 months. The pain and having to go to the bathroom is so bad. I can’t go anywhere. I wanted the transplant but they keep telling me it has to come back toxic cdiff if someone doesn’t help me soon I don’t think I am going to make. Please help
I had c-diff in 2012. I lost 7lbs in 3 days.
Was weak and my dr was a jerk. Said everything was in my head Switched drs.
Took 6 months and several rounds of Vancobto kill it. What worked was “pulsing” Vanco. This was at 6 months It worked this time!!! The spores know the Vanco routines of 7 days, next 10 days, etc. So the spore’s close their shell until the Vanco was finished. When the dr researched, he found that if
vanco is “pulsed” (made the treatment unpredictable) the spore would open it’s shell up and Vanco killed it! I can’t remember how the pulsing worked but was something like 1 Vanco, skip 2 or 3 days then take another dose which was also a varied dose (I don’t remember what the dose was ). Then the next dose was a different timing. Never the same.
Be sure to sterilize your bathroom and any area you use with bleach!!! So no one gets it and so you don’t get reinfected. Also keep your laundry separate and use some bleach. Florastore helped tremendously. Take it!!
I also went to Acupuncture. It helped in so many ways especially for the pain in my stomach, helped strengthen my immune system. Good luck!!
Florastor!! I was diagnosed with cliff a month back. Treated with vancomycin. I was better after a week and now I feel it coming back. Took 2 florastor this am an pm and it hasn’t gotten any worse.
Hi Jen, is Florastor an antibiotic or an over the counter item? I had my first c-diff infection 2 weeks after taking an antibiotic for a tooth problem. Was so bad that I was taken to hospital by ambulance and kept for 5 days. I was in Vancomycin 125 mg for 1o days, was good for a couple of days when it came back full force.
I’m back on Vancomycin for 4x a day for 10 days, 3x a day for 10 days, then 2 then 1 for 10 days. Total 100 capsules.
I can’t take a 4tf round of c-diff.
That’s why I’m questioning the Florastor, thanks!
Amy-Florastor is what will help along with the Vanco. Don’t be cheap and buy an off brand. I battled c diff for 3 years and FINALLY went away after I found florastor.
Florastor is the beast. 2- 250 mg a day will help your gut with c-diff and keep it right you are healed. I swear by it
Helpful article!! My mom was just diagnosed with a severe case of C.Diff and I’ve been on the hunt for the most specific probiotic to help with her condition
I’m on DOXYCYCLINE HYCLATE 100 for sinus and ear infection. Dr. said to take ACIDOPHILUS LACIOBACILLIUS with this because I had C-DIFF a couple of years ago. WILL THIS PREVENT ME FROM GETTING C-DIFF BACK FROM TAKING THE PROBIOTIC ?
Glad I came across this info. Diagnosed w cdiff without toxins yesterday. Started vancomycin but would like to get a yogurt that has probiotics that can help ease discomfort..Can you please recommend a yogurt? There are so many and I’m confused.
Thank You
Two Good or Belly’s should help of you can tolerate lactose.
I am 48 and tested positive in 2017 for Cdiff after taking antibiotics for an infected tooth. My doctor had me take many different combinations of medications and quite a few hospital stays to no avail. No medications helped me. After a 3 day visit in ICU at the hospital my doctor advocated for me to get a fecal transplant. I truly believe this saved my life. I was on my 5th treatment for this horrible bacteria. I had my good days and of course days when I didn’t know if I would survive. It’s nice to find a forum to hear other people’s stories and struggles
I’ve had c.diff now for eight months. I’m getting a fecal transplant next week. I’m so afraid of it not working. Any advice on what to eat after I’m home
Wondering if you can share your FMT experience. It’s something i’m very interested in, i live in Colorado. I have c-diff, SIBO, candida and hyppthyroid and don’t know what to do, what to treat first etc. Been going on for years! check out “breaking the vicious cycle” website about diet.
On 3rd reoccurrence of cdiff. My stomach hurts and is so bloated. Did you experience the stomach issue?
I had an FMT. Best thing I ever did. Mine was through colonoscopy. No issues and it worked immediately. I had tried Vanco many times and Dificid but it would return within two weeks every time. Hopefully you’ve sheet had the fmt and are healed.
Does the insurance cover the FMT?
I was told it could be done through an endoscopy/colonoscopy or by pill?
Hello I want to thank everyone for the information on cdiff. I’ve been dealing with CDiff for 9 months. I took Vancomycin & Cdeficid medicine and I finally said I’m not taking any more meds. So I stopped taking meds & I believe I no longer have it. My concern is what test can i take to prove that I no longer have cdiff? Any suggestion?
You have to pick up a kit from your doctor , follow directions to place stool in vial and return to doc or their lab.
I had to submit a stool sample to the la . Info mine came back positive again
Hi Annette. I am on my 3rd reocurrence of C Diff as well. I had slight abdominal pain and bloat due to the gas from the infection. I looked up natural ways to relieve gas online and came across simple yoga poses and stretches that help to pass gas. The bacteria release gas in your colon and it needs to be released.
If it gets worse, you should let your doctor know. How did you first contract C Diff? I got mine from antibiotics because my doctor thought I had a sinus infection when it was actually COVID. The combo of antibiotics killing my good bacteria and my low immunity from COVID just killed my gut hence the infection.
First occurrence was treated with Flagyl which was terrible. Came back after 2 days.
2nd occurrence was treated with 125mg Vancomycin 4X a day for 14 days. Started taking 500mg of Florastor after I finished and felt good for over a week. The symptoms did come back but they were mild.
I just tested positive for C Diff again but without toxins. My doctor just started me on a Vancomycin regimen again but it is tapered and pulsed. It starts with 125mg of Vancomycin 4X a day for 14 days, then twice a day for 7 days, then once a day for 7 days, then every 3 days for 8 weeks. I’m hoping it works. I will be taking Florastor during this regimen as advised by both my GI specialist and my pharmacist.
I hope you are feeling better
I have been on vanco for almost 2 weeks .Then I taper of every week .I have to take vanc for about a month and a half .I pray that the vanco will get rid of it for good .This is my 6th time of getting Cdiff in the last few years .If this does not work then I will have the fecal transplant .God Bless all of you .
My GI says FMT is no longer available. on my 4thround of CDiff since Jan. A nightmare. Taking Pulsed Vanco, Florastor, Vsl”3. Any and all to try to get rid of this.
Hi Paula,
Fecal transplant is available though not as widely as it once was. There have been two microbiome restoration therapies approved by the FDA recently, which work very similarly to an FMT. Rebyota is now available and can be performed in your doctor’s office. You can find out more information here: https://www.rebyota.com/
Hi, I have been battling C-Diff for at least 7 years with recurrences. I originally contracted it as a hospital patient after surgery for a ruptured small intestine and multiple IV antibiotics. I currently have a recurrence and awaiting treatment at Mass General with a fecal transplant. In 2019 I was hospitalized due to an electrolyte imbalanced caused by frequent diarrhea and was started on Vancomycin for about the 5th time. I was placed on a taper extending over 3 months. Soon after finishing the course noted that the hearing was lost in one ear which is irreparable. Please beware that this is a common side effect of Vanco. I am so grateful for the info regarding Florastor and will be purchasing it immediately. Meanwhile, I completed another 10 day course of Vanco and looking forward to the up-coming consultation at MGH. Best wishes to all in dealing with this most horrendous issue.
You don’t need a special post transplant diet. I ate regularly! Saved me physically and emotionally. I need to take an antibiotic and I’m petrified. Hope it never comes back. Glad I found this site! Good luck!
I got a horrible case of c. diff a few years back, (and then relapses). I’m still lactose intolerant and histamine intolerant (who knows what else). Came here looking for other probiotics to round out my gut. I’ve been taking VSL #3 for years. It was the only thing that let me not just lay in bed feeling like I just made out with a black hole. It’s really expensive, and you have to keep it fridged but check pharmacies for the off brand.. It worked just as good. It’s on Amazon but with the fridge thing, i didn’t trust it coming from online. Good luck everyone.
I contracted Cdiff this past summer and was very sick for about six weeks until I could get in to see the PA at a surgeon’s office who does colon rectal surgery. I told her that I was prescribed Clindamycin a few weeks before that. She had some tests done and sure enough I had Cdiff. I was given another milder antibiotic and got over it within two weeks, however I have IBS and I seem to get mucous more often from my colon. I take Align and was wondering if some other probiotic might help me overcome this better. The PA didn’t seem to know.
Orthobiotic is a very good probiotic for C-diff because it has Saccharomyces Boulardii in it. However, it is very expensive. If too pricey, there are other probiotics that contain this strain. I was told Orthobiotic is the best. I’m not sure about other brands.
I had C.diff in January 2020. I’ve taken Orthobiotic every day since. It is pricey, but I think it’s the best. (I am a pharmacist).
did not take antibiotic but got C.diff after 1 night in hospital,
10 days of Flagyl. Did not work alone.
Consulted compl med. who gave me a mixture chinese herbs, and 3 other products. Now a week later feel totally normal and hope it stays.
Recently treated with clindamycin
Since then severe diarrhea, stomach pain n mucus coming in stool. It’s c difficle . Can you please suggest and what herb mixture you have taken. And any effective probiotic. Any sort of advice can be helpful to me
Have had recurring cdiff for a year and a half. Likely never has left totally. After multiple treatments with dificid I had a 1 hr IV with zinplava and simultaneous 20 day dose of dificid. Still returning cdiff. Going for consult with Dr for fecal transplant. DK what else to do. My cdiff was caused by 4 surgeries for cancer with MANY antibiotics to follow. Clyndamyiacin was a killer. Anyone been through fecal transplant and have info??
What herbs did you use? Loosing faith in Western medicine, looking for other options.
Well, since this seems to be a current thread I’ll chime in to say that the only probiotic I found that contains S. Boulardii and also L Rhamnosis, which is also helpful for diarrhea, is Vitamin Bounty brand. I stumbled across it doing a google search and so far I feel like I guessed right. If it keeps helping me I’ll take it forever. I’m taking the lowest dose they have, 5 cfu.
My 4th bout with C-diff hit me today, exactly 1 week after finishing a tapered extended dose of Vancomycin. I have been taking Florastor for the past several months. Thinking of switching to the Bio K+, wondering if the liquid is more effective than pill form? I am desperate to get rid of this, I have been dealing with it since a MVA in August.
Would it make any difference to continue the Florastor and also take the Bio K+ along with it?
Seres 109 clinical phase 3 study you will get the real stuff and it will stop it ,
Omnibiotic AB10 HELPS AND FLORASTOR
Hi guys. I never re-tested for cdiff after getting it back in August of 2020 because my stools became formed while taking florastor but once I stopped my stools started losing its shape. Once I added florastor back in, my stool issue resolved. I really feel like it helps! Maybe not for all but it did for me. I believe I’m going through pi-ibs right now. I keep a food/stool journal and I’ve played around with different factors and I narrowed it down to florastor helping me.
I believe I have developed C. diff after nearly 4 weeks of antibiotic use. I am being tested and one result showed >3000 mcg Calprotectin (colitis). The doctor wants to do a colonoscopy but I read these are not necessary to diagnose C. diff??? I have been taking pharmacy grade probiotics for about 2 weeks and noticed considerable improvement. I am afraid the colonoscopy will exacerbate my colitis, especially if it is not necessary. Any thoughts on this?
Hi JC,
I would consult with your gastroenterologist in coordination with others who you see for your condition.
I felt it necessary for my patient, as did her GP & Neuro, to get a colonoscopy because the stool samples can eventually show as false negatives or false positives – even as soon as the second test if needed. Also, it was obvious to me & confirmed by her physicians that other digestive issues needed to be looked at and one colonoscopy could’ve handled all of this. She remained adamant in refusing to get one, which wasn’t uncommon behavior for her medically. That’s the only reason she didn’t have one – she refused “just because she could” and wouldn’t budge. There was no evidence that I could find nor her doctors to suggest it would exacerbate it.
I’ve had colonoscopies for stomach ulcers and it’s a quick yet effective procedure to look internally and assess innumerable things which in turn, helps provide a much quicker and thorough analysis of what’s going on and in turn, how to handle, steps to take, etc
Colonoscopies are excellent tools for this/C-diff and certainly colitis, and in looking into other things during the procedure.
Again though, I’d certainly talk with your gastroenterologist and your physician(s) whose care you’re in.
Good luck. I know it’s a tough time.
My doctor was able to diagnose me with c diff from stool samples. I did not need to get a colonoscopy.
After months of being on an antibiotic for an ear and tooth infection, I started having problems. I went to a GI and he immediately did a colonoscopy. I had told them about the antibiotic usage but totally disregarded testing me for cdiff. The colonoscopy was normal but my problems continued for months. I finally asked my primary to run a stool test and it was c diff. I was told by my primary and a different GI that c diff is not tested during a colonoscopy, only by stool sample. I am on my 6th reaccurance. I just bought Florastor after reading articles on this. I just wanted to reach out to people that if your GI jumps in on a colonoscopy before doing basic testing, ask them to please run stool samples first. I truly think that if the GI would have done this, I would not be going into my 6th month of reaccurance. That bacterial was in me for months when it could have been treated right away.
Seres 109 clinical trial
Who do I contact about this!
That trial is completed. You or your physician can ask for compassionate use by going here: https://www.serestherapeutics.com/patients-and-physicians/
Ask your doctor why he wants to do a colonoscophy. It will show problems in your intestines and you need to know if he is suspecting some problem.
Hi everyone,
I treated a patient who had MS & contracted C-diff during a short hospital stay for a septic UTI. I researched and experimented with every aspect on top of my diverse background as well as networking with other specialists, people who had it and/or were going through their repeat bouts with it, studies on C-diff, environmental factors and much more – what I really honed in on were the probiotics, diet, diarrhea, CDC guidance for contagious diseases and sanitizing and related to help resolve it and ideally, prevent reoccurrence.
I’ll note what I finally found to be effective regarding getting her C diff to go away in regard to antibiotics and probiotics vs all of the above.
Vancomycin was the only antibiotic that worked but not alone -no real progress was seen and she continued to have diarrhea and continual exacerbated digestive issues along with symptoms and issues throughout her body and system as a result. I added Florastar as the probiotic. But, the key to this or trick I found effective for this to really work and be effective was administering two probiotics to every single antibiotic. The antibiotic kept killing all of the bacteria in the gut. Two (probiotics) to one (antibiotic) – and, success finally.
Activia yogurt I found to be the best, and I made smoothies using it, fresh organic fruits, gatorade, etc (NO dairy is vital)….I got creative and taste tested all before. I ended up making them for me also they were that good. She got so bad, she was suffering from malnutrition. These smoothies were the only thing that helped while being tasty – she’s one who is extremely noncompliant medically overall but certainly with her diet, but she would drink these and they stuck whereas no other food or beverage would not. They would go straight through her system and cause more problems.
Very long story short –
After she was cleared (not sure how many months – the hospital discharged her much too soon so I was in charge from the time the hospital should have kept her in their care, but was once again neglectful unfortunately, and for at least five months, until I was finally able to get her clear of it… and approx her 5th test after original diagnosis).
Before I discharged her from my private care, I made sure her regular physician and neuro had a specific probiotic on her medication chart as a daily, vital, and lifelong one. They were excellent in working with me on this.
To keep it simple, just remember to double up on your probiotic during an episode and certainly if you’re taking an antibiotic. Otherwise, they should be taken as noted (usually once a day) when there’s no occurrence.
I now have it and if I’m without my probiotic for a day, wow. No good.
Yogurt that has no sugar and is dairy free is also an important addition.
Hope this helps.
Best wishes everyone
Doesn’t that kind of yogurt have way too much sugar in it to actually work?
Can you take the Florostar and the antibiotic at the same time or do they need to be separated?
Thank you
Hi Terri. I read that you should wait 2 hrs after antibiotic to take probiotics. I think this is to give the antibiotic time to move through your system and therefore be less likely to “kill” the probiotic
I am starting my second episode of c dificile. I drink lots of water and eat potatoes, cooked carrots and oatmeal. To healp my energy i drink 3 Boosts a day. Is Boost realy good for me?
Hi! I have had on going c diff for 4 months now! I was treated with vancomycin for 10 days my first infection but the infection came right back or didnt even clear up completely! I’m now on a tapering course of vancomycin, I have a month left on it! Please if anyone knows a good probiotic to help with my symptoms and all that! I still have horrible diaherra 4 weeks into treatment. Can barley eat or drink or leave my house..
Thank you!!
Get an FMT in the mean time seres 109 study.
Thank you all for your insight. My husband contacted CDiff while in the hospital for 4 mo with Covid He was on vancomycin for his Covid and ventilator pneumonia’s (+ a plethora of other infections). He’s had CDiff twice whine in the hospital and now has it for a third time We are worried he will build an immunity to vancomycin so now he’s switching to xifaxin. He needs a good probiotic so he can continue to recover and participate in therapy as he heals. Family is terrified we will contract it (my son thinks he does) Will consider all your input and advice. Thank you
Hi everyone, I have found Jarrows Formulas Saccharomyces Boulardii Plus MOS to be helpful. I take it everyday & its cheaper than florastor ( i get it on Amazon). Also, be careful with yogurt. The dairy can aggravate some people, and alot of yogurts have too much added sugar. Unfortunately, cdiff is something that seems like will always be with me. had my first episide w/ cdiff three years ago. I had been treated with antibiotics for frequent UTIs, so my dr. thinks this is how I contracted it. Unfortunately, it has recurred twice since than when Ive had to take an antibiotic for a UTI. I went to an infectious disease specialist who told me any time I have to take an antibiotic from now on, I will also have to take vancomycin to prevent the cdiff from returning. I just started coming down with another UTI today, and have started an antibiotics for that along w/ the vanco. Im doubling up on the probiotic too. I am very scared it will come back despite the vanco….I always keep clorox fuzion bleach spray & clorox germicidal cleaner on hand. After doing lots of research on what cleaner will kill the germs, these have proved to work. My greatest fear is if my family ever caught it. I wish you all the best, this is something I wouldn’t wish on anyone.
I was also told by an infectious disease doctor to go on vancomycin if I get prescribed an antibiotic. He also said that if I have to stay in the hospital for anything to let him know, and he may start me on vancomycin while I’m there. I continue to take Florastor daily because I was left with IBS symptoms following my first bout. I now take just 2 Forastor capsules a day instead of 4 that I started on.
Both of my bouts with CDIff were after hospital stays. I had a shoulder replacement a couple of years ago, but was not under the care of an infectious disease doctor, so developed CDIff again. I sure wish I had been under the care of this type of specialist. I had only seen gastro docs. So, I strongly urge anyone with this terrible illness to go to an infectious disease doctor and have them on board.
Amy, I went through multiple uti’s during peri menopause and discovered D-Mannose 500 mg and I take it religiously and haven’t had them any longer. Look into it, I hope it helps you. I’m looking at your Jarrow recommendation now for my c-diff. Thanks for sharing.
I have had Cd 4 times after 2 I had fecal Trans was good for 5 years just had it twice on a two month Va ncomycin and floroster feeling pretty good now.
I have the same prob w/recurring cdiff. Took antibiotics for uti’S then got cdiff. On vacomycin 3 weeks then again for 2 more weeks. Finally on divicid 10 days. Very expensive ..I paid $4900 for divicid 20 pills. So frustrating. Dr rx VSL 3 PROBIOTIC.
Did your husband have any trouble with dificid? They just started my husband on this. Yes, it is super expensive! Also, they want to give my husband zinplava with dificid. I haven’t read much about zinplava have you or did they talk about it to you.
Linda! Oh my gosh, your pharmacist did you a huge disservice. If you don’t have insurance, or your insurance refuses to cover Dificid, then many of the available pharmacy discount cards out there will cover it (Reducing the bill to around $900-1000 from $4900). However, if you insurance DOES cover Dificid (it usually only requires a Prior Authorization), AND you happen to have PRIVATE health insurance, then utilizing the manufacturer coupon lowers your bill to $50. ALWAYS do your research & NEVER trust your pharmacist. They are literally paid to do this and know this, but they don’t know or don’t care.
Good Rx, a discount card currently charges $4500.
Merck, the manufacturer will provide Rx at a discount or free if you are uninsured and basically indigent. My personal Medicare part D will cover 75% after deductible.
Not sure what the pharmacist could have done for the individual who posted.
I’ve been suffering from reoccurring C Diff due to antibiotic use back in January. I had symptoms of a sinus infection, Dr prescribed Amox then I found out I had COVID. Dr took me off Amox but damage had already been done. My compromised immune system from COVID combined with antibiotics killing all my good bacteria just wreaked havoc on my system.
I had a number of tests done on my stool in February but everything came up negative. I did have 2 types of protein detected, proteins that signify intestinal inflammation. My GI specialist scheduled a colonoscopy/endoscopy at the beginning of March to find out more. He took a stool sample and had it tested. Test came back positive. I was prescribed Flagyl 3X a day for 14 days which seemed to work but my symptoms came back 2 days after I finished.
I was then put on Vancomycin 4X a day for 14 days. It seemed to work a bit slower but I felt better after I finished. I was taking Phillip’s Colon Health while on the antibiotics but it did not seem to help.
I started taking Florastor right after I finished the Vancomycin and it seemed to help because I felt great for over a week. However, the symptoms did come back but not as severe.
Today I started a tapered/pulsed Vancomycin regimen which will take about 3 months to complete.
I will be taking Vancomycin 4X a day for 14 days, then 2X a day for 7 days, the 1X a day for 7 days, then 1 every 3 days for 8 weeks. I will also be taking Florastor so hopefully I can heal.
The only thing I have to deal with is the constant gas and bloating from the Florastor but have found yoga poses and stretches that can help release gas pressure naturally.
I also have a great dietician working with my GI specialist. She is researching different foods and probiotics that I can help me to recover faster and stop the weight loss. I have lost almost 25lbs because I have had to limit my food intake to foods that are gentle on my stomach. It has been a rough road.
What about consuming raw garlic and/or oil of oregano daily to prevent it kill c. Diff and MRSA?
One thing the doctors don’t talk about is that bad bacteria feed on sugar. Stop all sugar for at least 2 months after the antibiotics.
Excellent information here, thanks! I tried other supplements for months and finally found luck with Bio360. Most of their supplements have Lactobacillus and Bifido strains.
I had two bouts of c diff and took florastor , saccharmyces boulardie probiotic , ortho molecular bacillus coagulans , lactobacillus ,probulin and garden of life colon care ! I take four different strains every night .
I am doing much better and will continue this regimen.
I have had C diff for a year. Can’t get a Fecal Transplant yet, due to the fact they have a back log of patients needing them and they weren’t available due to Covid. I have been taking two different type of Probiotics. Florastor and one from Puritan Pride. I just finished taking Dificid since Vicomycin has not worked. I eat chobani yogurt, drink kefir and anything and everything to stop the C Diff from reoccurring. I have had bowel movements with straight blood, blood clots and had pain so bad I prayed I would die. I started throwing up and had to live with a bucket near my bed side. Finally they put me on Dificid. Dificid is a new antibiotic that can only be prescribed by the Infectious Disease Control Doctor. This is the most expensive antibiotic on the market. This antibiotic does kill all the good bacteria in your gut but attacks the bad bacteria. I still think I have C Diff and I’m still on the list for Fecal Transplant. Reading this article helped me decide which type of Probiotics to purchase. Bless all of you battling this horrible super bug. I hope all of you can survive this and good luck. Learn to eat healthy, eat lots of fermented foods and watch that sugar intake.
Omnibiotic AB10 IT HAS FACIUM AND LAURACIDIN
Which probiotic did you go with? Do you take culturelle?
My daughter was told to go on dificid. Thanks for providing information about that. I really appreciate any help.
Oh my gosh, I hope you are feeling much better now?
Correction on my post in regard to Dificid. Dificid kills the bad bacteria but not the good bacteria. I had no way of editing this. Just to let you all know.
I know this is accurate but it still confuses me regarding probiotic use and dificid. If it doesn’t kill the good….why is Florastor the only one recognized as helpful? I was first recommended it when I took Vancomycin and wondered if it’s still appropriate for Dificid.
Do you take the vancomycin and probiotic at the same time or separate??
Florastor is a yeast and not a bacteria; look it up on their website.
https://www.florastor.com/faqs.html
My mother had C. Diff at age 80. Florastor was what her GI told her to take and it worked wonderfully. The hospital had her on IV VANCOMYCIN when she was admitted for 3 days and when they released her with a prescription for oral Vancomycin, her pharmacist told her the copay was $1649.00. We panicked because she needed it desperately and we didn’t have the money to pay for it. I got on the internet and found a pharmacist chat site where some of the pharmacists advised me to find a compounding pharmacy and get the Vancomycin in an IV suspension and take it orally, that it would work the same way at a fraction of the cost. They were right. It didnt taste great but for only $42.00 out of pocket, we were thrilled. Just thought Id share that as a lot of people dont know that option exists.
Yes, It is very tough I am unable to find the best probiotic.
I had c diff after antibiotics 4 years ago and then had a relapse i used bio k plus and vsl 3 I finally got rid of c diff.
I also would make barley water and that was wonderful. You can look it up for recipes. Just boil barley in water and when soft drain the water (can add the barley to recipes to eat) then drink the barley water, it kinda tastes like oatmeal when you drink it. I liked it warm not cold and i swear by drinking this during c diff episodes and just any time to feel good.
I was told I needed to have c diff three times before I could get an FMT. I have collagenous colitis and have had diarrhea for years. I’m now on my second diagnosed bought of diarrhea. Did all of you who had success with FMTs have to wait?
Karen, yes! It was so frustrating. 9 months and 3 positive tests and they finally approved it.
I had a bout of Diverticulitis in early October (4th or 5th attack in 20 years). I was prescribed Augmentin. As always, it knocked out the diverticulitis. Two weeks later I started with unbearable cramps and bloody diarrhea. I was diagnosed with c diff and put on a 10 day regimen of Vancomycin. I also picked up Florastor and started taking 2 – 2x a day. After the Vancomycin ran out, I felt good for about a week. Stools were better despite some minor cramping still. Yesterday I was back in the ER. C Diff again! Another 10 days of Vancomycin. I will continue to take the Florastor because of the Saccharomyces boulardii. They have been studied and found effective against c diff. I found another probiotic that has shown to be helpful, too. It is called Lactobacillus reuteri. Is anyone else using this? What brand?
Yes, L. reutrei DSM 17938 strain is helping me from Bio Gaia, along w/ Florastor, Culrtuelle and Ideal Bowel Support from Jarrow
I found a probiotic on Amazon for the Lactobacillus reuteri it kills the bad bacteria for H. Pylori.
Last November I had COVID which primarily attacked my digestive tract. I have UC and both my GI doc and PCP told me COVID will attack weakest part of the body. Well my UC flared up, went into Diverticulitis, and then had C-Diff twice! And found out I am lactose intolerant! Lost so much weight as I couldn’t eat anything. Started taking lactobacillus reuteri-BioGaia-and what a difference it made! Now a year later am feeling great, have gained a little weight back (didn’t want to gain too much back????) and am eating pretty much anything-except for dairy that has lactose and stuff that irritates my UC.
My daughter has cdiff and this is the fourth time. She takes two culturelle a day. This cdiff occurred after taking antibiotics for strep throat. So, the family doctor prescribed dificid. Is this wise to take, considering she has had cdiff so often?
I am hoping someone out there can help, since I am waiting a referral for an adult GI doctor, she’s had an ultrasound (and nothing irregular was found), and we’ve been to the emergency center (who did bloodwork and a cat scan and found “a small amount of inflammation in the colon”).
What are your thoughts on dificid? She is 19.
Dificid is not an probiotic. It’s an antibiotic specifically for C. diff. It works to reduce recurrences by killing off only C. diff bacteria and leaving the other bacteria alone. It has been shown to reduce recurrences, so it’s a good option. Probiotics alone will not stop a C. diff infection, but they can be helpful in improving overall gut microbiome health and preventing future recurrences.
Thank you. Yes, we are working on getting this antibiotic filled. Apparently, our insurance company is battling with the doctor and us over whether this specific one is needed, since it is so expensive. I’m a teacher and my benefits are just “okay”, and I pay a lot for “okay”. Healthcare is just rough for everyone no matter what they do for a living. I was told this would be at least $450, which was with the insurance. I don’t care. It’s worth a try. I’ll do anything to help her. Thank you so much for your quick reply. I really appreciate it. I just wasn’t sure if we should put her on yet another antibiotic. The ER doctor said he would be hesitant, and her pediatric GI said since has not seen her in a bit, she couldn’t make that call, but the family doctor was pushing the Dificid. I just am not sure what to do. It’s so frustrating. I will be asking this adult GI doctor (since my daughter is now 18 and can no longer see the peds one) what probiotics will help. We are waiting for a call back on a referral. My daughter takes Culturelle now and has been for years.
Does your body change over time and would it need a different type of probiotic?
I am so happy I stumbled on this forum. I read all of the posts and replies and I feel like I have learned so much even from this page alone. Thank you to everyone who posted and thank you for replying. I am learning in hopes that I can help my daughter as much as possible. They have suggested the fecal implantation, and reading the posts about that has helped me as well.
Thank you!
As I mentioned in a comment that I just posted above, I would suggest getting an infectious disease doctor on board. Good luck to your daughter. This illness shook my world and I’m a senior.
Which probiotic did you go with? Do you take culturelle?
My daughter was told to go on dificid. Thanks for providing information about that. I really appreciate any help.
58 yo healthy Male, vegetarian. I had surgery a little over 2 weeks ago and have had symptoms of C.diff. since day 2 post-surgery. Diarrhea every day since, feels like inflamed bowels, etc.
As suggested; I started the Florastor today and bought a bunch of non-dairy yogurts.
My biggest questions; do I have a chance to knock this out with this regimen or am I going to have to go through a Vanco treatment?
Thanks for any help & insight.
You should be tested if you are having symptoms. Same thing happened to me…I was in the hospital for 5 days and had diarrhea when I left hospital. One week later I was back in the ER with a bad case of C. Diff. I’m on Vancomycin now and hoping I will not have a recurring case. I’m supposed to have another surgery this week but am scared to death about it making the C.Diff worse.
Chris I would first do a stool test to see if you do have C.diff or not. If you’ve had surgery to your bowel it could be diarrhea from that or it could be from C.diff but get a stool test to see what the problem actually is.
As for Vancomycin I’ve been on it 2 times for C.diff recurrences. I looked up the drug and it doesn’t kill the spore but only the toxins and so even thou its a go to drug its still isn’t good enough! And Flagyl (metronidazole) I took another time and all I could think of was Projectile Vomiting but did complete the course. I ended up using my boyfriend’s do-do and did an at home FMT but after a year I think I may have C.diff back again for the 4th time. I just had a blood test done which showed elevated White Blood Cells & Lymphocytes but will get a stool test after the weekend to find out for sure.
I think with the recurrence in many of the patients on here it shows that there needs to be better and newer treatments available. In my situation I have proven that antibiotics are not really a successful answer to the problem. I’m thinking that flooding the colon with sterile H20 and then sucking it all out may be a good tactic before adding any FMT and or probiotics.
I think the infection may reoccur due to unkilled spores hiding inside the bowel. They likely sit in there until an opportune time to start producing their toxins again and creating havoc. It’s either that or folks are unknowingly reinfecting themselves due to spores left in their environment. I would say some good scientific detective work would help to answer that.
I have a question…
Can anyome tell me if I should be taking Florastor or BioK while I’m taking Vancomycin? Or is it better to take it AFTER completing my vancomycin? I can’t seem to find the answer to this on this page and I’ve read every post. Did I miss it? Thank you for your help.
Hello Kathleen,
May I ask how did it go with taking the amoxicillin?
I have a small issue where they want me to take an antibiotic too when I battled cliff for as long as you did with fecal transplant and I take florastor too. Thank you for your help in advance.
Hi Daisy, how did vancomycin work for you. I’ve been dealing with this for 3 weeks, just found out it was Cdiff a week ago. Deathly afraid of the antibiotics and it’s side effects.
Also to anyone who may read this, is vancomycin or antibiotics the only way to beat this for sure..my symptoms are mild. Rib stomach pain, small appetite, bloating loose stool
This is a useful information for people with Cdiff. Thank you for sharing.
Anyone try FMT capsules? If so did you order online or get from a local gi doctor. Seems like it would be easy to administer to a 93 year old that is currently in hospital with cdiff again. Hospital does not do FMT so I guess I have to get pills and administer. They have been on Vancomycin for about 2 months, I think they stopped it and it came back with a vengeance.
Please let me know what helped your 93 year old mother. My mom is the same age.
My wife has a C diff, but somehow she still manages it, only that she has lots of health problem sometimes, a migrane, bloated stomach, etc.
Please put me on email list
I took a capsule of Florastor and made yogurt with it.
This way I know my yogurt will have the proper probiotic in it. It also proves that the probiotic in the Florastor is alive.
I think I will order some of the Bio K plus and also add that in the next time I make yogurt.
Just heat the milk to about 117 degrees (about 2 cups) put it into a mason jar, open up the probiotic capsule and add it and put the lid on the jar and shake well to incorporate. Then you need to keep it fairly warm for a good 12 plus hours until it cultures and sets. Put this jar in the fridge for when you make a larger batch of yogurt. I make a gallon at a time and you need about 3/4 of a cup of start for a gallon. I have an ice chest that I put hot water in and then put my container of milk plus starter into the warm water with a lid on it. You don’t need to cover the jar or container, just enough hot water to hold the milk warm. Cover the ice chest and the water stays warm all night or all day.
Made real good yogurt and I know it’s the right strain.
Thank you all so so much ♥️♥️♥️
I had a problem with my digestion before because of unhealthy eating, but when I started eating probiotic foods and supplements, my problem with my digestion started to vanish. Thanks for posting content about probiotics. This is a valuable article. Great post!
I’m a 34 year old healthy nurse. I ended up getting cdiff from the hospital I work at. It was terrible but vancomycin worked immediately. My last vancomycin was 2 weeks ago. I started taking jarrow 100 10 billion cfu. But then came across this article. Should I start taking the florastor? Or is it too late? If so how long? I feel great since taking the jarrow “gut balance” . I’ve asked drs and they don’t seem to know much about probiotics.